Karl L. R. Jansen, M.D., Ph.D. is a Member of the Royal College of Psychiatrists and is the world’s leading expert on ketamine. He has studied ketamine at every level. While earning his doctorate in clinical pharmacology at the University of Oxford, he photographed the receptors to which ketamine binds in the human brain. He has published papers on his discovery of the similarities between ketamine’s psychoactive effects and the near-death experience (NDE) during his study of medicine in New Zealand. Dr. Jansen believes that ketamine can have potent healing powers when used as an adjunct to psychotherapy but warns of the addictive nature of ketamine. Because of this risk, he has developed new methods for the treatment of ketamine addiction. Dr. Jansen left Oxford in 1993 to train in psychiatry at the Maudsley and Bethlem Royal Hospitals. Dr. Jansen welcomes correspondence on the topic of ketamine. He can be contacted via e-mail at k@btinternet.com. Recent ketamine studies have shown how the brain completely shuts down during the “K-Hole” out-of-body experience.
1. Dr. Jansen’s Research Subject’s Near-Death Experience
The following is an excerpt from Dr. Karl Jansen’s book, Ketamine: Dreams and Realities, where he documented one man’s NDE and how it is nearly identical to a ketamine experience he had a week later. The man lost his wife in a tragic fire and had the NDE while trying to rescue her.
I had an NDE about 6 days before the first time I took ketamine because my then partner died. She had a party at her flat and the flat caught fire. I got out of the flat and thought that she was out as well, but she’d been really drunk and she’d slipped and fallen and pushed the room door shut. I got out and shouted, “Christ, she’s not here!” and went back up. The flat was full of thick smoke. I thought, “Right, what you do is you get down on the floor and crawl along the corridor.” But there was no air there. I crawled along and couldn’t see anything. I could hear her and I was trying to push open this door but I couldn’t. I was overcome with smoke, and clink!
The next thing it was like white light and then everything going very fast. All these sounds and things sounding far off and very close and far off, then whoosh! You’re out of your body and there was all this light. All this sounds really crap, like one of those 1940s Old Testament films … It all happened so quickly. The next thing, it’s very bright, you’re out of your body, flying through the night and there’s light, there’s light. Er, well, it’s pitch black and there’s light – that’s a better way of describing it.
You go into the light and you just feel that everybody who has ever died is there. Not heavenly choirs as such, but there’s certainly a lot of people around you and you get waves of concern. And the next thing was swoosh! And it was back to the everyday world very quickly. When I came back it was so abrupt, and I was fine really – I had a very narrow escape. Your first impression would be that you fly up in the air but that can’t be. I’d have laughed at myself ten years ago for saying this kind of thing.
So I had an out-of-body experience and then I got hauled out of the flat by ambulance guys who put an oxygen mask on my face. My partner was on a life-support machine from the Saturday until Monday, when they switched the machine off.
2. Dr. Jansen’s Research Subject’s Ketamine Experiences
I had acquired the “K” (ketamine) a week previously for the party, but didn’t do it until a few days after she died. It was the first time I had taken “K”.
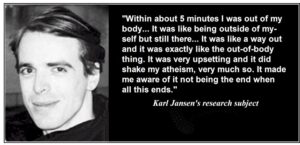
I had the flat to myself. Everybody was out and I sat in the front room on a big comfy chair and just took this stuff. Within about 5 minutes I was out of my body. I was still numb after what had happened. It was like being outside of myself but still there.
I could smell this perfume she used to wear. I could sense her all round me. It was like a way out and it was exactly like the out-of-body thing. It was very upsetting and it did shake my atheism, very much so. It made me aware of it not being the end when all this ends.
I tried “K” again quite a number of times and the same thing happened every time. It was like this pure consciousness. I hadn’t any shape. You could fly and you could actually travel although you are still in the same place. You are in the place where everybody is who has ever died. It’s this big entity. It’s not like an old guy with a beard. It’s this sense of energy that everybody who has ever moved on is there together and it was like she was looking after me. Precisely the same thing happened with the “K” as happened in the (burning) flat, which to someone not expecting it would be pretty scary. It was exactly the same.
I thought that I would never find anybody again and why hadn’t I died as well, why hadn’t I managed to get her out of that room? I thought it was my fault, I blamed myself for ages. I had a half-hearted idea of taking loads of pills and not waking up but what’s the point in that? I’ve already been to that place once and they wouldn’t have me then, so why would they have me the second time?
Concerned friends and parents made me go into counseling and therapy and to see psychiatrists. I was put onto various things like Prozac, but I was finding that my own “extra treatment” (the ketamine) was doing me a lot more good because “K” is very cathartic. I was doing it because it made me feel better, except the first time when it was quite a shock. It made me feel a lot less unhappy knowing that she was still there in one way or another. It would have taken a lot longer for me to recover if I hadn’t taken “K” because it gets rid of a lot of hurt instantly … It’s very reassuring in a way.
3. Does Ketamine Produce Near-Death Experiences?
It is possible that Ketamine HCL (Ketalar, Vetalar, Ketaset) can induce NDEs. Dr. Karl Jansen has extensively researched this topic and links to his work can be found at the bottom of this page. The following is a summary of articles on the Internet concerning Ketamine as related to NDEs.
Ketamine is an anesthetic that is available only to physicians and is “scheduled” in several states. Since anaesthetizing levels of Ketamine “knock you out”, the dose required to have an experience is 6 to 10 times smaller than what is given by veterinarians and physicians. “Ketamine is a prescription only medicine and so is not covered by the Misuse of Drugs Act. This means that possession of ketamine is not a criminal offense. However, under the Medicines Act, unauthorized supply is illegal.”
Tunnels, experiencing God (even if it is you) and oneness, meeting others, out-of-body experiences, life-changes (including “values”), sometimes frightening experiences, seeing the future, experiencing a true reality, believing that you have died, and experiencing things that words cannot describe are all common elements of Ketamine and NDE experiences.
The life-changing aspects of Ketamine are so strong that research in Russia claims that it is very effective in curing alcoholism, phobias, depression, and neuroses. Yale received approval to conduct a double-blind study to confirm the Russian research as it relates to alcoholism. The Russian researcher (Dr. Evgeny Krupitsky) has recently received $24,000 to study the effectiveness of Ketamine in curing heroin addicts.
4. Dr. Evgeny Krupitsky’s Ketamine Research
A dose of 50 mg (.7 mg/kg) induces a motion picture of colored images when eyes are closed. When eyes are open, ordinary reality remains but assumes an unusual air. Orientation is resolved. On 100-150 mg (1.4-2.1 mg/kg) ordinary reality disappears even when eyes opened. Perceptions of one’s own body also disappear. The subject discovers himself as a point of consciousness which moves in very strange worlds yet the feeling of self remains. On doses higher than 150 mg (2.1 mg/kg) intramuscularly, the feeling of individual self dissolves. The process of losing one’s individuality can be horrifying and felt as a real death. If the subject can relax and let go, this process may be ecstatic. After the loss of the feeling of one’s individual self, the experience is indescribable. There exists only “That which is aware of Itself.”
The changes in the Minnesota Multiphasic Personality Inventory (MMPI) after Ketamine Psychedelic Therapy (KPT) session testified to positive personality changes. Changes in the Color Test of Attitudes after KPT testified to a positive transformation of the unconscious emotional attitudes of our alcoholic patients towards themselves and their significant others. Changes in our Spirituality Scale testified to a significant increase in the level of spiritual development after the ketamine session. All these psychological changes favored sober life. As a rule, we also observed positive transformations in our patients’ systems of life values, purpose and meaning, but these changes had not been previously measured quantitatively with psychological tests. Clinical impressions and indirect evidence from the Spirituality Scale suggested these changes, but not a rigorous scientific proof.
5. Examples of Ketamine Induced NDE experiences
These comments were taken out of context, but it gives you a sense of how similar the experiences can be. I complained to Dr. Karl Jansen (the only researcher I am aware of that is concerned specifically with Ketamine as it relates to NDEs) that the Ketamine experiences have similar qualities, but my overall impression is that they are not as profound and centered on love. He replied that the setting of the experience makes a lot of difference. Taking a recreational drug in your house is much different from being in a hospital or other sudden situation where you may be in pain or afraid that you are about to die. Here are some excerpts:
Example 1: “Looooooovvvvvvvveeeeeeeeeee, Reeeaaaalllliiiiittttyyyyyyyy, Hoooommmmmeeeee. I was God, I saw light and warmth. This is Home. Sooo familiar, where we belong. Where we go. Everything is perfect, no words, just basic feeling. Love, Reality, Home. This was about the only words that I could bring back. Really no words there, but strong feelings. I Knew I was God and that I wasn’t a little while before, but didn’t have any idea what I was before. I was completely calm and comfortable, it was Home. Perfect. I wasn’t alone either.
Example 2: “(Buzzing occurred) Most of the time I felt like a pure light that could flow like lava and make sweet guitar-distortion sounds, I was burning very bright. I could just ‘be’ in this state, it felt beautiful. Other times I would have conscious thoughts, I would note that I felt godlike, I would love myself, it was great. When I’d think of my friends I’d feel very warm, but the couple times I tried explaining to them how I was feeling (I had to get up and piss quite a few times, was still dizzy), I felt the words totally inadequate, and I’d lose the feeling.”
Example 3: “(Buzzing occurred) Tunnel vision and a feeling of ‘being deep inside your own body’ occurs.”
“Reality as we normally experience it had crumbled into a different form. It was as though the world broke up, revealing another dimension. The subject was there, and not there at the same time – there was no apparent boundary between the subject and object – the world and I became one … Although it was certainly an extreme experience, it was fundamentally unsatisfying. No real insight into the world, or even the experience were gained,
Example 4: “Bubbles, bouncing babies and bubbles, she kept saying.
“I can’t feel my body anymore except this overriding general fuzziness. The lines on the ceiling become a tunnel and I am flying down it faster than sound approaching the speed of light…
“Oh no, the tunnel takes a big dive downwards! I am facing straight down this big tunnel and I am falling. . . .
“Now there are rules. I can see them all. I am outside my room looking down at us and I know all the rules. There is so much going on outside of us. Other people, other rules, other things, that we are not allowed to see in the day to day. More knowledge. Who is next to me. What is next to me. I know it is something important. I say who is there.”
Example 5: “One friend of mine who took it thought he had died, but he wasn’t frightened or upset by this at all, which should give you some indication of just how weird things can get.”
Example 6: “It sort of dissociates you from your live. I drifted trough worlds of other dimensions from inside the cosmos towards the outside of the circular thing which is called the universe.(Sounds strange, but that is what I felt) I also had the feeling that I have learned a lot of spiritual things. It is perhaps truth, there was not especially much fun. But I was satisfied and content as I would be after a long adventure holiday.”
Example 7: “I realized then that I didn’t travel between theses two worlds but only shifted my attention in a different direction. I always was and probably always will be in this world I found there, but living different lives I will enter different ‘simulations’.”
“I floated back with a peaceful and content feeling. I felt that I had experienced something good, something special. I was slowly entering my body, like putting on a garment: legs first, then arms, chest, head. At the same time, my sight and hearing returned as I was shifting my attention to these senses. Everything felt a bit unreal at first, but this went away after a while.
“This experience felt to me as real as anything I know from this world. Now, three Months later this hasn’t changed. I consider this level possibly dangerous for unexperienced users, because of the strong impact it has on your life. In my case, experiencing reality as ‘just a game‘ could have easily driven me into suicide, if I wasn’t happy with this life.”
They have been reported as spending a great deal of time analyzing conversations that they have held with the various Ketamine entities. These beings offer great insights into life, the universe and everything. In the words of one such traveler into the realm of the hyper-real, “It is no great accomplishment to hear a voice in the head. The accomplishment is to make sure that it is telling you the truth.”
6. How Dangerous is Ketamine?
Although most of the comments on this page about Ketamine are positive, and it is routinely used as an anaesthetic in much larger doses, Ketamine is not a safe drug. For example, you can pass out, vomit, and suffocate. Depending on your source, you may not know how large a dose your are taking. If I understand some of the user’s comments correctly, it seems that Ketamine may produce substantially negative and long-lasting psychological effects, bringing to mind fears of LSD trips that can ruin your life. Here are some of the negative comments about Ketamine experiences:
a. Comment #1: “People who have taken the drug report a range of effects from the unpleasant, to the downright dangerous. Reports from America offer numerous examples of users who get trapped in repeated, compulsive administration of the drug giving rise to incidents usually associated with bad acid trips, with people believing that they can fly or attempting to get out of moving vehicles. Others have suffered paranoia or severe delusional states. In the last few months, it has been increasingly evident that such incidents are no longer limited to the USA. Having the Ketamine entities lie to us may be the least of our worries.”
b. Comment #2: “In fact, though I may be wrong on this, I would consider such an adventure to be a high risk one. Please be careful.”
c. Comment #3: “Not a bad idea to have a straight person around while you’re doing it, especially if there are open flames nearby or anything like that. Like I said, you’ll be very out of it.”
d. Comment #4: “After my experience with ketamine, I was advised, and agreed, to take a semester off from school. I was warned that I might experience flashbacks. I did not.
“I awoke from the anaesthesia to the the most petrifying, unpleasant experience of my life. I experienced hallucinations that were beyond description. I, also, experienced severe memory loss … I was unable to recognize family and friends. I was, also, very anxious and restless. I said things that made no sense. According to the attending anaesthesiologist, I was “insane” for five days. The attending, later, went to NIH to brief the doctors, there, of my reaction.
“My family and I were later told that my reaction was worse than the norm, but certainly not atypical. I have always been surprised that this drug is still available, but I understand it does have positive pediatric and vet. uses.
“As a result of my experience, though, I would would certainly wonder why anyone would wish to experiment with ketamine. That is only one persons opinion, though.”
e. Comment #5: “[Ketamine experiences] are possibly dangerous for unexperienced users because of the strong impact it has on one’s life. In my case, experiencing reality as ‘just a game’ could have easily driven me into suicide, if I wasn’t happy with this life.”
It is significant that 30 percent of normal subjects given ketamine insisted that they had not been dreaming or hallucinating, but that the events had really happened.
7. The Ketamine Model of the Near-Death Experience by Karl Jansen
a. About the Author
Dr. Karl Jansen was born in New Zealand and trained in medicine at the University of Otago. After registering as a medical practitioner, he proceeded to carry out brain research at the University of Auckland as a research fellow of the New Zealand Medical Research Council. At this time he became interested in ketamine and its effects and published his first observations in this area, and also in antipodean use, users and consequences of psilocybin-containing mushrooms. He then went to the United Kingdom, and attended the University of Oxford (New College) were he completed a Doctor of Philosophy in Clinical Pharmacology. He was the Glaxo Fellow at Green College. On completion of his studies at Oxford, he went to the Maudsley Hospital and London Institute of Psychiatry to complete his training as a psychiatrist. He is now a member of the Royal College of Psychiatrists. His current research interests are the ketamine model of the near-death experience and the consequences of long-term, high dose recreational use of Ecstasy (MDMA).
He would like to receive correspondence concerning the subject of this paper.
Dr. Jansen has the following to say about the journal article that follows:
‘I am no longer as opposed to spritual explanations of these phenomena as this article would appear to suggest. Over the past two years (it is quite some time since I wrote it) I have moved more towards the views put forward by John Lilly and Stan Grof. Namely, that drugs and psychological disciplines such as meditation and yoga may render certain ‘states’ more accessible. The complication then becomes in defining just what we mean by ‘states’ and where they are located, if indeed location is an appropriate term at all. But the apparent emphasis on matter over mind contained within this particular article no longer accurately represents my attitudes. My forthcoming book ‘Ketamine’ will consider mystical issues from quite a different perspective, and will give a much stronger voice to those who see drugs as just another door to a space, and not as actually producing that space’.
b. Abstract
Near-death experiences (NDE’s) can be reproduced by ketamine via blockade of receptors in the brain (the N-methyl-D-aspartate, NMDA receptors) for the neurotransmitter glutamate. Conditions which precipitate NDE’s (hypoxia, ischaemia, hypoglycaemia, temporal lobe epilepsy etc.) have been shown to release a flood of glutamate, overactivating NMDA receptors resulting in neuro (‘excito’) toxicity. Ketamine prevents this neurotoxicity. There are substances in the brain which bind to the same receptor site as ketamine. Conditions which trigger a glutamate flood may also trigger a flood of neuroprotective agents which bind to NMDA receptors to protect cells, leading to an altered state of consciousness like that produced by ketamine. This article extends and updates the theory proposed in 1990 (Jansen, 1990b).
c. Introduction
The near-death experience (NDE) is a phenomenon of considerable importance to medicine, neuroscience, neurology, psychiatry, philosophy and religion (Stevenson and Greyson, 1979; Greyson and Stevenson, 1980; Ring, 1980; Sabom, 1982; Jansen, 1989a,b, 1990b). Unfortunately, some scientists have been deterred from conducting research upon the NDE by claims that NDE’s are evidence for life after death, and sensationalist media reports which impart the air of a pseudoscience to NDE studies. Irrespective of religious beliefs, NDE’s are not evidence for life after death on simple logical grounds: death is defined as the final, irreversible end. Anyone who ‘returned’ did not, by definition, die – although their mind, brain and body may have been in a very unusual state.
There is overwhelming evidence that mind results from neuronal activity. The dramatic effects on the mind of adding hallucinogenic drugs to the brain, and the religious experiences which sometimes result, provide further evidence for this (Grinspoon and Bakalar, 1981). One of the many contradictions which ‘after-lifers’ can not resolve is that “the spirit rises out of the body leaving the brain behind, but somehow still incorporating neuronal functions such as sight, hearing, and proprioception” (Morse, 1989, original italics).
All features of a classic NDE can be reproduced by the intravenous administration of 50 – 100 mg of ketamine (Domino et al., 1965; Rumpf ,1969; Collier, 1972; Siegel,1978, 1980,1981; Stafford, 1977; Lilly, 1978; Grinspoon and Bakalar, 1981; White, 1982; Ghoniem et al., 1985; Sputz, 1989; Jansen, 1989a,b, 1990b, 1993). There is increasing evidence which suggests that the reproduction of NDE’s by ketamine is unlikely to be a coincidence. This evidence includes the discovery of the major neuronal binding site for ketamine, known as the phencyclidine (PCP) binding site of the NMDA receptor (Thomson et al., 1985), the importance of NMDA receptors in the cerebral cortex, particularly in the temporal and frontal lobes, the key role of these sites in cognitive processing, memory, and perception, their role in epilepsy, psychoses, hypoxic/ischaemic and epileptic cell damage (excitotoxicity), the prevention of this damage by ketamine, the discovery of substances in the brain called ‘endopsychosins‘ which bind to the same site as ketamine, and the role of ions such as magnesium and zinc in regulating the site (Anis et al., 1983; Quirion et al., 1984; Simon et al., 1984; Benveniste et al., 1984; Ben-Ari,1985; Thomson, 1986; Coan and Collingridge, 1987; Collingridge, 1987; Contreras et al., 1987; Rothman et al., 1987; Mody et al., 1987; Quirion et al., 1987; Westbrook and Mayer, 1987; Sonders et al., 1988; Barnes,1988; Choi,1988; Monaghan et al., 1989; Jansen et al., 1989a,b,c, 1990a,b,c, 1991a,b,c, 1993).
d. Characteristic Features of the Near-Death Experience
There is no internationally determined and agreed set of criteria which define the NDE, no list of ‘research diagnostic criteria’ similar to those provided by the American Psychiatric Association (APA) for psychiatric disorders. This lack has allowed some critics of neurobiological models to dismiss these models because some particular criterion which they believe to be important may not have been fully accounted for by the model being proposed, although it may well be that a consensus, statistical definition of the key features of the NDE would not include those features – just as, for example, the APA definition of schizophrenia (1980) represents an international consensus and avoids the sectarian views of a few, or inclusion of obscure cases which do not meet the general rule. For example, Gabbard and Twemlow (1989) argued that Saavedra -Aguilar and Gomez-Jeria’s neurobiological hypothesis (1989), which was based on temporal lobe electrical abnormalities, did not have general validity because Gabbard and Twemlow had identified 5 cases in which hypoxia and stress did not appear to be a triggering factor (temporal lobe epilepsy, and many acute psychoses, can occur spontaneously without any apparent triggering factors). These cases are certainly not adequate grounds for the dismissal of neurobiological models.
Ketamine administered by intravenous injection, in appropriate dosage, is capable of reproducing all of the features of the NDE which have been commonly described in the most cited works in this field, and the following account is based upon these (Domino et al., 1965; Rumpf, 1969; Collier, 1972; Siegel,1978, 1980, 1981; Stafford, 1977; Lilly, 1978; Grinspoon and Bakalar, 1981; White, 1982; Ghoniem et al., 1985; Sputz, 1989; Jansen, 1989a, b,1990b, 1991c, 1993). Important features of NDE’s include a sense that what is experienced is ‘real’ and that one is actually dead, a sense of ineffability, timelessness, and feelings of calm and peace, although some cases have been frightening. There may be analgesia, apparent clarity of thought, a perception of separation from the body, and hallucinations of landscapes, beings such as ‘angels‘, people including partners, parents, teachers and friends (who may be alive at the time), and religious and mythical figures. Transcendant mystical states are commonly described. Memories may emerge into consciousness, and are rarely organized into a ‘life review‘ (Greyson, 1983).
Hearing noises during the initial part of the NDE has also been described (Noyes and Kletti, 1976a; Morse et al., 1985; Osis and Haraldsson, 1977; Greyson and Stevenson, 1980; Ring, 1980; Sabom, 1982). Ring (1980) classified NDE’s on a 5 stage continuum: 1. feelings of peace and contentment; 2. a sense of detachment from the body; 3. entering a transitional world of darkness (rapid movements through tunnels: ‘the tunnel experience’); 4. emerging into bright light; and 5. ‘entering the light’. 60% experienced stage 1, but only 10% attained stage 5 (Ring, 1980). As might be expected in a mental state with a neurobiological origin, more mundane accounts also occur, e.g. children who may ‘see’ their schoolfellows rather than God and angels (Morse, 1985). It is clear that NDE’s are not as homogeneous as some have claimed.
e. Ketamine and Phencyclidine
Ketamine is a short-acting, hallucinogenic, dissociative anaesthetic related to phencyclidine (PCP). Both drugs are arylcyclohexylamines – they are not opioids and are not related to LSD. In contrast to PCP, ketamine is relatively safe, an uncontrolled drug in most countries, and remains in use as an anaesthetic for children (White et al., 1982). Anaesthetists attempt to prevent patients from having NDE’s (emergence phenomena) by the co-administration of benzodiazepines and other sedative substances which produce ‘true’ unconsciousness rather than dissociation (Reich and Silvay, 1989).
Ketamine produces an altered state of consciousness which is very different from that of the ‘psychedelic’ drugs such as LSD (Grinspoon and Bakalar, 1981). It can reproduce all features of the NDE, including travel through a dark tunnel into light, the conviction that one is dead, ‘telepathic communion with God’, hallucinations, out-of-body experiences and mystical states (see ketamine references above). If given intravenously, it has a short action with an abrupt end. Grinspoon and Bakalar (1981, p34) wrote of: ‘…becoming a disembodied mind or soul, dying and going to another world. Childhood events may also be re-lived. The loss of contact with ordinary reality and the sense of participation in another reality are more pronounced and less easily resisted than is usually the case with LSD. The dissociative experiences often seem so genuine that users are not sure that they have not actually left their bodies.’
A psychologist with experience of LSD described ketamine as ‘experiments in voluntary death’ (Leary, 1983, p375). Sputz (1989, p65) noted: ‘one infrequent ketamine user reported a classic near-death experience…”I was convinced I was dead. I was floating above my body. I reviewed all of the events of my life and saw a lot of areas where I could have done better”. The psychiatrist Stanislav Grof stated: “If you have a full-blown experience of ketamine, you can never believe there is death or that death can possibly influence who you are” (Stevens, 1989, p481-482). ‘Ketamine allows some patients to reason that … the strange, unexpected intensity and unfamiliar dimension of their experience means they must have died..’ (Collier, 1981, p552).
Attempts to explain NDE’s as hallucinations are sometimes rejected by spiritualists because many persons insist upon the reality of their experiences (Osis and Haraldsson, 1977; Ring, 1980). However, 30% of normal subjects given ketamine were certain that they had not been dreaming or hallucinating, but that the events had really happened (Rumpf et al., 1969; see also Siegel, 1978). What is a hallucination?: “a hallucination has the immediate sense of reality of a true perception … transient hallucinatory experiences are common in individuals without mental disorder” (APA, 1980). The apparently clear sensorium of some persons who have had NDE’s has also been used to argue that the NDE is ‘real’ and not a hallucination (Osis and Haraldsson, 1977; Ring, 1980). It is thus important to note that hallucinations in schizophrenia typically occur in clear consciousness and are believed to be real (APA, 1980). A personal conviction of the ‘reality’ of an NDE does not invalidate scientific explanations. Some users of LSD have claimed that their minds are clearer than usual, and that the LSD world is real while the ‘normal’ world is a veil of illusion (Grinspoon and Bakalar, 1981). Cardiac arrest survivors have been reported as describing their resuscitation in detail (Sabom, 1982). Ketamine can permit sufficient sensory input to allow accounts of procedures during which the patient appeared wholly unconscious (Siegel, 1981).
f. Glutamate, NMDA and Sigma Receptors, and the Hippocampus
Most large neurones in the cerebral cortex use glutamate as their neurotransmitter. Glutamate, an excitatory amino acid, is central to the function of the hippocampus, temporal and frontal lobes (Cotman et al., 1987; Fagg and Foster, 1983; Greenamyre et al., 1984; Monaghan, Bridges and Cotman, 1989; Jansen et al., 1989c, 1990a) and plays a vital role in all cognitive processes involving the cerebral cortex, including thinking, memory and perception (Monaghan, Bridges and Cotman, 1989; Oye et al., 1992).
The major neuronal binding site for ketamine is called the PCP receptor, which is itself attached to the NMDA receptor (Monaghan, Bridges and Cotman, 1989). As they are part of the same macromolecular complex, the two terms are sometimes used interchangeably. It was formerly believed that the sigma and PCP sites were the same entity, but it is now clear that sigma receptors are very different, have a unique distribution in the CNS, and are not a form of opioid receptor (Walker et al., 1990; Jansen et al., 1991b) .
There was initially some debate as to whether the hallucinogenic properties of ketamine were due to NMDA or sigma receptors (Jansen, 1990b). These effects are now largely attributed to NMDA receptor blockade (Krystal et al., 1994). Sigma ligands with a high degree of specificity (e.g. (+)pentazocine) do not produce NDE’s at doses where most of the binding is to sigma rather than NMDA and/or kappa opioid receptors (sigma receptor ligands frequently have affinity for NMDA and/or kappa opioid receptors at higher doses) (Musacchio et al., 1990; Walker et al., 1990).
When glutamate is present in excess, neurones die via a process called excitotoxicity. Conditions which have been proven to lead to excessive release of glutamate include hypoxia/ischaemia, epilepsy and hypoglycaemia (e.g. Rothman, 1984; Rothman and Olney, 1986, 1987). Blockade of PCP receptors prevents cell death from excitotoxicity (e.g. Rothman et al., 1987). The brain may thus have a protective mechanism against a glutamate flood: release of a counter-flood of substances which block PCP receptors, preventing neuronal death. Considering the sophistication of the brain’s many known defences, and the vulnerability of neurones to hypoxia, a protective mechanism against excitotoxicity seems very likely. This is the only speculation in the process outlined above: the other statements are strongly supported by experimental evidence (Benveniste et al.,1984; Simon et al., 1984; Ben-Ari, 1985; King and Dingledine, 1986; Rothman et al., 1987; Westerberg et al., 1987; Hoyer and Nitsch, 1989). A peptide called a-endopsychosin, which binds to the PCP receptor, has been found in the brain (Quirion et al., 1984). Certain ions such as magnesium and zinc also act as endogenous PCP channel blockers (Thomson, 1986; Westbrook and Mayer, 1987; Cotman, Monaghan and Ganong, 1988), and it is possible that these ions are centrally involved in producing NDE’s.
g. Scientific Hypotheses and NDEs
Claims that NDE’s must have a single explanation (e.g. Ring, 1980), or that a scientific theory must explain all of the experiences ever given the name of NDE (e.g. Gabbard and Twemlow, 1989) are difficult to justify. It is well established that mental phenomena have multiple causes and variable expressions. The NDE is more likely to be the final common expression of several different causes. Even then, the final ‘common’ expression contains sufficient variability to suggest different types of NDE, for example in Ring’s study (1980), only 10% ‘enter the light’. A multi-levelled interpretation is thus the most useful. The glutamate hypothesis of the NDE is not intended to apply to every NDE, and is not necessarily incompatible with the theories described below.
h. Temporal Lobe Epilepsy
It has been claimed that there is some similarity between the phenomena experienced in temporal lobe epilepsy (TLE) and NDE’s (Persinger and Makarec ,1987; Saavedra-Aguilar and Gomez-Jeria,1989). Glutamate is the key neurotransmitter in the temporal lobe, particularly in the hippocampus, and is implicated in epilepsy. The neuropathology of epilepsy is believed to result from excito-toxic cell death (Ben-Ari, 1985; King and Dingledine, 1986; Olney, Collins and Sloviter, 1986; Mody and Heinemann, 1987; Cotman, Monaghan and Ganong, 1988).
A neuroprotective system might become active in any excitotoxic situation including epilepsy. The degree of damage, and the mental state, resulting from a glutamate flood may depend on the final balance in each neuronal pathway between excito-toxic forces and neuroprotective mechanisms. Persons who were oxygen deprived for prolonged periods and had a profound NDE, sometimes survived the episode unimpaired (Sabom, 1982). The lack of apparent brain damage may result from a very effective mechanism for glutamatergic blockade in those individuals.
It is also possible that ketamine has its effects by mimicking some of the pathological processes seen in temporal lobe epilepsy. Even though ketamine blocks glutamatergic transmission, and prevents excitotoxic cell death, the effect of ketamine upon the human electroencephalograph (the EEG) suggests that it can be epileptogenic – the final result of ketamine acting in the brain is the result of a complex interplay of forces. There is a reduction in a wave activity, but b, d and q wave activity are increased (Schwartz et al. 1974; Pichlmayr et al., 1984). Ketamine acts both as an anticonvulsant (e.g. McCarthy et al., 1965; Celesia and Chen, 1974; Taberner, 1976; Leccese et al., 1986; Mares et al., 1992) and as a pro-convulsant (Bennet et al., 1973; Gourie et al., 1983; Myslobodsky, 1981). Myslobodsky (1981) reported that ketamine could produce epileptiform EEG patterns in human limbic and thalamic regions, but that there was no evidence that this affected other cortical regions or that fits were likely to occur. This is consistent with the NDE model presented by Saavedra-Aguilar and Gomez-Jeria (1989) involving limited electrical abnormalites in the limbic system. Thus production of NDE’s by ketamine is not at odds with proposals that NDE’s may result from abnormal electrical activity. Reich and Silvay (1989): ” it is hard to draw objective conclusions regarding the anti-convulsant properties of ketamine…animal data are particularly difficult to interpret because of interspecies variations”. Ketamine is probably anticonvulsant at NDE producing doses (Myslobodsky, 1981) suggesting that a PCP receptor blocker is released to produce the NDE.
i. A Flood of Endorphins
Carr (1981, 1989) proposed that NDEs resulted from a flood release of endogenous opioids (endorphins). It had been reported that survival time was increased by giving opiate antagonists (e.g. naloxone) in fatal circumstances (Holoday and Faden, 1978). More recently, a sudden increment of b-endorphin has been reported in the brain and body fluids of dogs who are ‘conscious’ at the moment of death (Sotelo et al., 1995). It is now known that a glutamate flood results in excitotoxic cell death in hypoxia/ischaemia and epilepsy (see above). However, glutamate is an amino acid. Endorphins are unlikely to produce NDE’s as they are not potent dissociative hallucinogens (Oyama et al., 1980). Injection of b-endorphin into the CSF has analgesic effects lasting well over 22 hours (Oyama et al.,1980). This does not match the time course of a typical NDE which is relatively brief. Ketamine produces brief, deep analgesia (White et al., 1982) due to NMDA (PCP) receptor blockade ( e.g. Schouenberg and Sjolund, 1986; Parsons et al., 1988). The limited psychotomimetic properties of some opioids (e.g. (-) pentazocine) result from binding to k opioid receptors, and to PCP receptors at higher doses (Pfieffer et al., 1986; Mussachio et al., 1990). However, the effects of (-)pentazocine binding to k receptors, at doses which are relatively selective, are described as ‘feelings of cheerfulness and strength’ (Belville and Forrest, 1968), a description bearing no resemblance to the dramatic effects of ketamine or NDE’s. With higher doses, more marked effects may appear as a result of binding to PCP receptors – but pentazocine is not an endorphin. Claims that sigma- selective (+)isomers of benzomorphan opiates have psychotomimetic effects are not generally supported by human trials, carried out in the 1960’s, which demonstrated that it is the (-)isomers which have psychotomimetic properties – and these may prefer PCP receptors rather than sigma sites (review: Mussachio,1990). The naloxone-reversible component is due to k opioid receptor binding, while the naloxone insensitive component is due to PCP (i.e. NMDA) receptor binding, not sigma binding (Walker et al., 1990). The role of opioid receptors in ketamine effects is contoversial (Reich and Silvay, 1989). Naloxone could not reverse the effects of ketamine in humans (Amiot et al., 1985) and dogs (Vaupel, 1983). However, ketamine is supplied as a racemic mixture of (+)and (-) isomers. The controversy may be resolved by studying the separate effects of the isomers, and the doses at which these appear. As doses rise, drugs bind to a wider range of receptors. Ketamine can induce NDE’s at doses about four times less than those required for anaesthesia (Stafford, 1977; Lilly, 1979; Grinspoon and Bakalar, 1981; Sputz, 1989). White et al. (1980) reported that it was (+)ketamine which has some opioid binding properties and which produced the most anaesthesia, while (-)ketamine produced more NDE’s (described by anaesthetists as ‘psychic emergence reactions’). White et al. (1985) went on to show that (+)ketamine is about four times more potent as a hypnotic and analgesic, and has different effects upon the EEG.
Saavedra-Aguilar and Gomez-Jeria (1989) cited animal experiments showing b-endorphin to be epileptogenic to support an argument that b-endorphins produce NDE’s (e.g. McGinty et al., 1986; Henriksen et al., 1978). While b-endorphin may have had these effects within the rat paradigms used, opioids usually produce calming, inhibitory effects in humans – not excitation or states resembling epilepsy (Meltzer, 1987). Released peptides probably have protective functions rather than contributing further to excito-toxicity. The finding of Su, London and Jaffe (1988), that some steroids bind to sigma receptors, was cited to suggest that steroids could play a role in NDE’s. However, the steroid was progesterone which is not a hallucinogen. Schwartz et al. (1989) reported that the affinity of progesterone for the sigma site is insufficient to result in significant receptor occupancy, except in pregnancy.
j. Hypoxia and Hypercarbia
Hypoxia
Blacher (1980) suggested that hypoxia induced NDE’s. This has been criticised by some authors (Sabom, 1982) as studies involving a slow fall in inspired oxygen produced mental clouding rather than NDE’s (Henderson et al., 1927). However, these studies are not an accurate model of events in, for example, cardiac arrest. Sudden hypoxia causes an excessive release of glutamate with resulting excitotoxicity, which can be prevented by ketamine (see previous references).
Hypercarbia
A CO2-enriched breathing mixture can result in typical NDE phenomena such as bodily detachment and the perception of being drawn towards a bright light. Diverse personality types produced broadly similar reports, suggesting a shared neurological substrate (Meduna, 1950).
k. Serotonin
Like endorphins, serotonergic effects may be contributory but are unlikely to play a central role in the NDE. Psychedelic drugs such as LSD are serotonergic in action and produce a mental state very different from NDE’s . There is frequently an overwhelming increase in sensory input from the external environment (Grinspoon and Bakalar, 1981), in contrast to the dissociation produced by ketamine. Psychedelic visual phenomena bear little relationship to the dream-like images of ketamine and the NDE. ‘Ego dissolution’ experienced on LSD has a different quality from the conviction of having died which may arise with ketamine. Loss of contact with the external environment leading rapidly to the ‘tunnel experience’ is not a typical psychedelic drug effect, although it may occur.
l. Psychological
a. Depersonalisation: The NDE may be an adaptive mechanism which alerts one to the threat of death while potentially overwhelming emotion is held at bay. The reality can then be integrated without panic (Greyson, 1983; Noyes and Kletti, 1976a,b). This model is applicable when death is psychologically near as when falling from a cliff. While protecting nerve cells from excitotoxicity is then irrelevant, glutamate and NMDA receptors would be involved in producing the experience as they play a key role in cognition and perception.
b. Regression in the service of the ego: confronting death cuts off the external world resulting in regression to a pre-verbal level. This is experienced as mystical ineffability (Greyson, 1983). Losing contact with the external world is one of the most typical effects of ketamine. This is partially due to blockade of NMDA receptors involved in sensory transmission. NMDA receptors play a central role in the transmission of data from all sensory modalities (Davies and Watkins, 1983; Greenamyre et al., 1984; Headley et al., 1985; Cotman et al., 1987; Cline et al.,1987; Monaghan, Bridges and Cotman, 1988; Kisvardy et al., 1989; Oye et al., 1992).
c. State dependant reactivation of birth memories (Grof and Halifax, 1977). Movement through tunnels towards light may be a memory of being born : a ‘near-birth experience‘. NMDA receptor blockade could be the mechanism for such a reactivation of primitive memories.
d. Sensory deprivation: memories may normally be suppressed by a ‘gate’ which admits primarily external signals when we are fully conscious and concentrating upon an external task (Siegel,1980, 1981). If this input is dramatically reduced (e.g. by ketamine or a heart attack) in combination with central stimulation (e.g. by excessive glutamate release during hypoxia, epilepsy, or arising without external provocation), stored perceptions are released and become ‘organized’ into a meaningful experience by psychodynamic forces in the mind in question (Greyson, 1983). The ‘white light’ may result from CNS stimulation , and also a possible lowering of the phosphene perceptual threshold (Siegel,1980, 1981). Sensory deprivation can produce profound alterations in consciousness (Lilly, 1961,1978).
The hippocampus is the anatomical location of the ‘memory gate’ described above. NMDA receptors form the molecular substrate of the gate. NMDA receptors have their highest concentration in the hippocampus, a part of the medial temporal lobe where data from the external world is integrated with internal programs. The NMDA receptor plays an important role in learning, and in the formation and retrieval of memories. The PCP receptor is referred to as a ‘gated channel’. Whether the gate is open or closed depends on the degree of excitation – specifically, the position of a magnesium ion in the channel. In simple terms, ketamine blocks this channel and closes the gate to incoming data (Monaghan, Bridges and Cotman, 1989; Morris et al., 1986; Collingridge, 1987; McNaughton and Morris, 1987; Cotman, Monaghan and Ganong, 1988).
m. Drug-induced hallucinations?
Administered drugs may explain some cases of NDE’s, but in most no drugs were given with effects of this nature (Sabom, 1982).
n. Conclusions
NDE’s can be safely induced by ketamine, and the glutamate theory of the NDE can thus be investigated by experiment. Discoveries in neuroscience suggest a common origin for ketamine experiences and the NDE in events occuring at glutamatergic synapses, mediated by NMDA receptors via their PCP channel component. This hypothesis links most of the neurobiological and psychological theories (hypoxia, a peptide flood, temporal lobe electrical abnormalities, regression in the service of the ego, reactivation of birth memories, sensory deprivation etc.) rather than being an alternative to them. Most of the tenets of the hypothesis are strongly supported by experimental evidence which implicates glutamate and NMDA receptors in the processes which precipitate NDE’s. The postulate that anti-excitotoxic agents can flood the brain remains to be clearly established.
Spiritualists have sometimes seen scientific explanations of NDE’s as dull and reductionist. However, the exploration of the mind-brain interface is one of the most exciting adventures which humans have ever undertaken. The real reductionism lies in attempts to draw a mystical shroud over the NDE, and to belittle the substantial evidence in favour of an scientific explanation.
o. References
American Psychiatric Association (1980). Diagnostic and Statistical Manual of Mental Disorders, Third Edition, APA, Washington, DC.
Amiot, J. F., Boujou, P. and Palacci, J. H. (1985). Effect of naloxone on loss of consciousness induced by iv ketamine (letter). British Journal of Anaesthetics, 57, 930.
Anis, N.A., Berry, S. C., Burton, N. R. and Lodge, D. (1983). The dissociative anaesthetics ketamine and phencyclidine, selectively reduce excitation of central mammalian neurons by N methyl-aspartate. British Journal of Pharmacology, 79, 565 – 575.
Barnes, D. M. (1988). NMDA receptors trigger excitement. Science, 239, 254 – 256.
Ben-Ari, Y. E. (1985). Limbic seizure and brain damage produced by kainic acid: mechanisms and relevance to human temporal lobe epilepsy. Neuroscience, 14, 375 – 403.
Bellville, J. and Forrest, W. (1968). Respiratory and subjective effects of d- and l- pentazocine. Clinical Pharmacology and Therapeutics, 9, 142 – 151.
Bennett, D. R., Madsen, J. A. and Jordan, W. S. (1973). Ketamine anesthesia in brain damaged epileptics. Neurology (Minneapolis), 23, 449-450.
Benveniste, H., Drejer, J., Schouseboe, A. and Diemer, H. H. (1984). Elevation of the extracellular concentrations of glutamate and aspartate in rat hippocampus during cerebral ischaemia monitored by microdialysis. Journal of Nuerochemistry, 43, 1369 – 1374.
Blacher, R. S. (1980). The near death experience. Journal of the American Medical Association, 244, 30.
Carr, D. B. (1981). Endorphins at the approach of death. Lancet, 1, 390.
Carr, D. B. (1989). On the evolving neurobiology of the near-death experience (PDF). Journal of Near- Death Studies, 7, 251 – 254.
Celesia, G. G. and Chen, R. (1974). Effects of ketamine on EEG activity in cats and monkeys. Electroencephalography and Clinical Neurophysiology 37, 345-353.
Choi, D. W. (1988). Glutamate neurotoxicity and diseases of the nervous system. Neuron, 1, 623 – 634.
Cline, H. T., Debski, E. and Constantine-Paton, M. (1987). NMDA receptor antagonist desegregates eye specific stripes. Proceedings of the National Academy of Sciences, 84, 4342 – 4345.
Coan, E. J. and Collingridge, G. L. (1987). Effects of phencyclidine, SKF10,047 and related psychotomimetic agents on N-methyl-D-aspartate receptor mediated synaptic responses in rat hippocampal slices. British Journal of Pharmacology, 91, 547 – 556.
Collier, B. B. (1972). Ketamine and the conscious mind. Anaesthesia, 27, 120 – 134.
Collingridge, G. L. (1987). The role of NMDA receptors in learning and memory. Nature, 330, 604 – 605.
Cotman, C. W. and Monaghan, D. T. (1987). Chemistry and anatomy of excitatory amino acid systems. In: Meltzer, H. Y., Psychopharmacology: The Third Generation of Progress(1987) pp197 – 218.
Cotman, C. W., Monaghan, D. T., Ottersen, O. P. and Storm-Mathisen, J. (1987). Anatomical organisation of excitatory amino acid receptors and their pathways. Trends in Neurosciences, 10, 273 – 279.
Cotman, C. W., Monaghan, D. T. and Ganong, A. H. (1988). Excitatory amino acid neurotransmission: NMDA receptors and Hebb-type synaptic plasticity. Annual Review of Neuroscience, 11, 61-80.
Davies, J. and Watkins, J. C. (1983). Role of excitatory amino acid receptors in mono and polysynaptic excitation in the cat spinal cord. Experimental Brain Research, 49, 280 – 290.
Domino, E. F., Chodoff, P. and Corssen, G. (1965). Pharmacologic effects of CL-581, a new dissociative anaesthetic, in man. Clin. Pharmacol. Therapeutics, 6, 279- 291.
Fagg, G. E. and Foster, A. C. (1983). Amino acid neurotransmitters and their pathways in the mammalian central nervous system. Neuroscience, 9, 701-771.
Foster, A. and Fagg, G.E.,(1987). Taking apart NMDA receptors. Nature, 329, 395
Gabbard, G. O. and Twemlow, S. T. (1989). Comments on ‘A neurobiological model or near-death experiences‘. Journal of Near-Death Studies, 7, 261 – 264.
Ghoneim, M. M,, Hinrichs, J. V., Mewaldt, S. P. and Peterson, R. C. (1985). Ketamine: behavioral effects of subanaesthetic doses. Journal of Clinical Psychopharmacology, 5, 70-77.
Gourie, D. M., Cherian, L. and Shankar, S. K. (1983). Seizures in cats induced by ketamine hydrochloride anaesthesia. Indian Journal of Medical Research, 77, 525-528.
Greenamyre, J. T., Young, A. B. and Penney, J. B. (1984). Quantitative autoradiographic distribution of l-[3H]glutamate binding sites in rat central nervous system. Journal of Neuroscience, 4, 2133-2144.
Greyson, B and Stevenson, I. (1980). The phenomenology of near-death experiences. American Journal of Psychiatry, 137, 1193-1200.
Greyson, B. (1983). The psychodynamics of near-death experiences. Journal of Nervous and Mental Disease, 171, 376 -380.
Grinspoon, L. and Bakalar, S. B. (1981). Psychedelic Drugs Reconsidered. Basic Books, New York.
Grof, S. and Halifax, J. (1977). The Human Encounter With Death. E. P. Dutton, New York.
Headley, P. M. , West, D. C. and Roe, C. (1985). Actions of ketamine and the role of N-methyl aspartate receptors in the spinal cord: studies on nociceptive and other neuronal responses. Neurological Neurobiology, 14, 325 -335.
Henderson, Y. and Haggard, H. W. (1927). Noxious gases and the Principles of Respiration Influencing their Action. American Chemical Society, New York.
Henriksen, S. J., Bloom, F. E., McCoy, F., Ling, N. and Gullemin, R. (1978). B-endorphin induces non-convulsive limbic seizures. Proceedings of the National Academy of Sciences, 75, 5221-5225.
Holaday, J. W. and Faden, A. L. (1980). Naloxone reversal of endotoxin hypotension suggests role of endorphins in shock. Nature, 275, 450-451.
Hoyer, S.. and Nitsch, R. (1989). Cerebral excess release of neurotransmitter amino acids subsequent to reduced cerebral glucose metabolism in early-onset dementia of Alzheimer type. Journal of Neural Transmission, 75, 226-232.
Jansen, K. L. R. (1989a). The near-death experience. British Journal of Psychiatry , 154, 882-883.
Jansen, K. L. R (1989b). Near-death experience and the NMDA receptor. British Medical Journal, 298, 1708 – 1709.
Jansen, K. L. R., Faull, R. L. M. and Dragunow, M. (1989c). Excitatory amino acid receptors in the human cerebral cortex: a quantitative autoradiographic study comparing the distribution of [3H]TCP, [3H]glycine, l-[3H]glutamate, [3H]AMPA and [3H]kainic acid binding sites. Neuroscience, 32, 587-607.
Jansen, K. L. R., Faull, R. L. M. and Dragunow, M. and Synek, B. (1990a). Alzheimer’s disease: changes in hippocampal N-methyl-D-aspartate, quisqualate, neurotensin, adenosine, benzodiazepine, serotonin and opioid receptors – an autoradiographic study. Neuroscience, 39, 613-617.
Jansen, K. L. R. (1990b). Neuroscience and the near-death experience: roles for the NMDA-PCP receptor, the sigma receptor and the endopsychosins. Medical Hypotheses, 31, 25 – 29.
Jansen, K. L. R. (1990c). Ketamine: can chronic use impair memory? International Journal of Addictions, 25, 133 – 139.
Jansen, K. L. R. and Faull, R. L. M. (1991a). Excitatory amino acids, NMDA and sigma receptors: a role in schizophrenia? Behavioral and Brain Sciences, 14, 34-35.
Jansen, K. L. R., Faull, R. L. M., Dragunow, M. and Leslie, R. (1991b). Autoradiographic distribution of sigma receptors in human neocortex, hippocampus, basal ganglia, cerebellum, pineal and pituitary glands. Brain Research, 559, 172-177.
Jansen, K. L. R. (1991c). Transcendental explanations and the near-death experience. Lancet, 337, 207-243.
Jansen, K. L. R (1993). Non-medical use of ketamine. British Medical Journal, 298, 4708-4709.
King, G. L. and Dingledine, R. (1986). Evidence for the activation of the N-methyl-D- aspartate receptor during epileptic discharge. In: Excitatory Amino Acids and Epilepsy (eds. R. Schwarz, Y. Ben-Ari) pp520-570, Plenum, New York.
Kisvardy, Z. F., Cowey, A., Smith, A. D. and Somogyi, P. (1989). Interlaminar and lateral excitatory amino acid connections in the striate cortex of monkey. Journal of Neuroscience, 9, 667-682.
Krystal, J. H., Karoer, L. P., Seibyl, J. P., Freeman, G. K., Delaney, R., Bremner. J. D., Heniger, G. R., Bowers, M. B. and Charney, D. S. (1994) Subanesthetic effects of the noncompetitive antagonist, ketamine, in humans. Archives of General Psychiatry, 51, 199-214.
Leary, T. F. (1983) Flashbacks, an autobiography. J. P. Tarcher, L. A., p375.
Leceese, A. P., Marquis, K. L., Mattia, A. and Moreton, J. E. (1986). The anticonvulsant and behavioral effects of phencyclidine and ketamine following chronic treatment in rats. Behavioral Brain Research, 22, 257-233.
Lilly, J. C. (1961). Experiments in solitude, in maximum achievable physical isolation with water suspension, of intact healthy persons. In: Physiological aspects of Space Flight. pp 238-247, Columbia University Press, New York.
Lilly, J. C. (1978). The Scientist: A Novel Autobiography. Bantam Books, J. B. Lippincott, New York.
Lobner, D. and Lipton, P. (1990). Sigma ligands and non-competitive NMDA antagonists inhibit glutamate release during cerebral ischaemia. Neuroscience Letters, 117, 169-174.
MacDonald, J. F., Miljkovic, Z. and Pennefather, P. (1987). Use dependant block of excitatory amino-acid currents in cultured neurons by ketamine. Journal of Neurophysiology, 58, 251-265.
Mares, P., Lansitiakova, M., Vankova, S., Kubova, H and Velisek, L. (1992). Ketamine blocks cortical epileptic afterdischarges but not paired-pulse and frequency potentiation. Neuroscience, 50, 339-344.
Mayer, M. L. , Westbrook, G. L. and Guthrie, P. B. (1984). Voltage-dependent block by Mg2+ of NMDA receptors in spinal cord neurons. Nature, 309, 261 -263.
McCarthy, D. A., Chen, G., Kaump, D. H. and Ensor, C. J. (1965). General anaesthetic and other pharmacological propperties of CL-581. Journal of New Drugs, 5, 21-33.
McGinty, J. F., Kanamatsu, T., Obie, J. and Hong, J. S. (1986). Modulation of opioid peptide metabolism by seizures: differentiation of opioid subclasses. NIDA Research Monographs, 71, 89 – 101.
McNaughton, B. C. and Morris, R. G. M. (1987). Hippocampal synaptic enhancement and information storage within a distributed system. Trends in Neurosciences, 10, 408- 415.
Meduna, L. J. (1950). The effect of carbon dioxide upon the functions of the brain. In: Carbon Dioxide Therapy (Meduna, L. J., ed.) , Charles Thomas, Ill., pp23-40.
Meldrum, B. S. (1987). Protection against hypoxic /ischaemic brain damage with excitatory amino acid antagonists. Medical Biology, 65, 153 – 157.
Meltzer, H. Y. (1987). (ed). Psychopharmacology: The Third Generation of Progress. Raven Press, New York.
Mody, I. and Heinemann, U. (1987). NMDA receptors of dentate gyrus cells participate in synpatic transmission following kindling. Nature, 326, 701-703.
Monoghan, D. T., Bridges, R. J. and Cotman, C. W. (1989). The excitatory amino acid receptors. Their classes, pharmacology and distinct properties in the function of the nervous system. Annual Review of Pharmacology and Toxicology, 29, 365-402.
Morris, R. G. M., Anderson, E., Lynch, G. S. and Baudry, M. (1986). Selective impairment of learning and blockade of EPT by NMDA antagonist AP5. Nature, 319, 744-776.
Morse, M., Conner, D. and Tyler, D. (1985). Near death experiences in a paediatric population. American Journal of Diseases of Children, 139, 595-563.
Morse, M. L. (1989). Comments on ‘A neurobiological model for near-death experiences’. Journal of Near-Death Studies, 7, 223-228.
Mussacchio, J. M. and Klein, M. Canoll, P. D. (1990). Dextrometorphan sites, sigma receptors and the psychotomimetic effects of sigma opiates. Progress in Clinical Biological Research, 328, 13-16.
Myslobodsky, M. S., Golovchinsky, V. and Mintz, M. (1981). Ketamine: convulsant or anticonvulsant? Pharmacology, Biochemistry and Behavior, 14, 27-33.
Nowak, L., Bergestovski, P., Ascher, P., Herbet, A. and Prochiantz, A. (1984). Magnesium gates glutamate-activated channels in mouse central neurons. Nature, 307, 462-465.
Noyes, R. and Kletti, R. (1976a). Depersonalisation in the face of life threatening danger: a description. Psychiatry, 39, 19 – 30.
Noyes, R. and Kletti, R. (1976b). Depersonalisation in the face of life threatening danger: an interpretation. Omega, 7, 103-108.
Olney, J. W., Collins, R. C. and Sloviter, R. S. (1986). Excitotoxic mechanisms of epileptic brain damage. Advances in Neurology, 44, 857-877.
Osis, K. and Haraldsson, E.(1977). At the hour of death. Avon, New York.
Oyama, T.Y., Jin, T., Yamaga, R., Ling, N. and Guillemin, R. (1980). Profound analgesic effects of beta-endorphin in man. Lancet, 1, 122-124.
Oye, N., Paulsen, O. and Maurset, A. (1992). Effects of ketamine on sensory perception: evidence for a role of N-methyl-D-aspartate receptors. Journal of Pharmacology and Experimental Therapeutics, 260, 1209-1213.
Parsons, C. G., Gibbens, H., Magnago, T. S. I and Headley, P. M. (1988). At which sigma site are the spinal actions of ketamine mediated? Neuroscience Letters, 85, 322-328.
Persinger, M. A. and Makarec, K. (1987). Temporal lobe epileptic signs and correlative behaviors displayed by normal populations. Journal of General Psychology, 114, 179-195.
Pichlmayr, l., Lips, U. and Kunkel, H. (1984). The Electroencephalogram in Anaesthesia. Berlin: Springer-Verlag; pp102-105.
Peters, S., Koh, J. and Choi, D. W. (1987). Zinc selectively blocks the action of N- methyl-D-aspartate on cortical neurons. Science, 236, 589-592.
Pfieffer, A., Brantl, V., Herz, A. and Emrich, H. M. (1986). Psychotomimeis mediated by k opiate receptors. Science (Washington, DC), 233, 774-776.
Quirion, R., Chicheportiche, R., Contreras, P. C., Johnston, K,. M., Lodge, D., Tam, S. W. Woods, J.H., and Zukin, S. R. (1987). Classification and nomenclature of phencyclidine and sigma receptor sites. Trends in Neurosciences, 10, 444 – 446.
Quirion, R., Dimaggio, D. A., French, E. D., Contreras, P. C., Shiloach, J., Pert, C. B., Evert, H., Pert, A. and O’Donohue (1984). Evidence for an endogenous peptide ligand for the phencyclidine receptor. Peptides, 5, 967-977.
Rauschecker, J. P., Hahn, D. (1987). Ketamine-zylazine anaesthesia blocks ` consolidation of ocular dominance changes in kitten visual cortex. Nature, 326, 183-185.
Reich, D. L. and Silvay, G. S. (1989). Ketamine: an update on the first twenty-five years of clinical experience. Canadian Journal of Anaesthetics, 36, 186-197.
Ring, K. (1980). Life at death: a scientific investigation of the near death experience. Coward, McCann, Goeghegan; New York.
Rothman, S.M. (1984). Synaptic release of excitatory amino acid neurotransmitter mediates anoxic neuronal death. Journal of Neuroscience, 4, 1884-1891.
Rothman, S.M and Olney, J. W. (1986). Glutamate and the pathophysiology of hypoxic/ischaemic brain damage. Annals of Neurology, 19, 105-119.
Rothman, S.M and Olney, J. W. (1987). Excitotoxicity and the NMDA receptor. Trends in Neurosciences, 10, 299-302.
Rothman, S.M., Thurston, J. H., Hauhart, R. E., Clark, G. P. and Solomon., J. S. (1987). Ketamine protects hippocampal neurons from anoxia in vitro. Neuroscience, 21, 673 – 683.
Rumpf, K., Pedick, J., Teuteberg, H., Munchhoff, W. and Nolte, H. (1969). Dream-like experiences during brief anaesthesia with ketamine, thiopental and propiadid. In: Ketamine (ed. H. Dreuscher) pp 161-180, Sprigner-Verlag, Berlin.
Sabom, M. B. (1982). Recollections of death: a medical investigation. Harper and Row, New York.
Saavedra-Aguilar, J. C. and Gomez-Jeria, J. S. (1989). A neurobiological model of near-death experiences. Journal of Near-Death Studies, 7, 205-222.
Schoenberg, J. and Sjolund, B. H. (1986). First order nociceptive synapses in rat dorsal horn are blocked by an amino acid antagonist. Brain Research, 379, 394-398.
Schwartz, M. S., Virden, S. and Scott, D. F. (1974). Effects of ketamine on the electroencephalograph. Anaesthesia, 29, 135-140.
Schwarz, S., Pohl, P. and Zhou, G. -Z. (1989). Steroid binding at sigma ‘opioid’ receptors. Science (Washington, DC), 246, 1635-1637.
Siegel, R. K. (1978). Phencyclidine and ketamine intoxication: a study of recreational users. In: Phencyclidine Abuse: An Appraisal. (ed. R. C. Peterson and R. C. Stillman) pp119 – 140, National Institute on Drug Abuse Research Monograph 21. NIDA, Rockville, Maryland.
Siegel, R. K. (1980). The Psychology of life after death. American Psychologist, 35, 911-950.
Siegel, R. K. (1981). Accounting for after-life experiences. Psychology Today 15, 67.
Simon, R. P., Swan, S. H. , Griffiths, T. and Meldrum, B. S. (1984). Blockade of NMDA receptors may protect against ischaemic damage in the brain. Science, 226, 850-852.
Sloviter, R. S. (1983). “Epileptic” brain damage in rats induced by sustained electrical stimulation of the perforant path. Brain Research Bulletin, 10, 675 – 697.
Sotelo, J., Perez, R., Guevara, P. and Fernandez, A. (1995). Changes in brain, plasma and cerebrospinal fluid contents of b-endorphin in dogs at the moment of death. Neurological Research, 17, 223 – 225.
Sputz, R. (1989). I never met a reality I didn’t like: A report on ‘Vitamin K’. High Times, October 1989, 64-82.
Squire, L. R. and Zola-Morgan, S. (1988). Memory: brain systems and behavior. Trends in Neurosciences, 11, 170-175.
Stafford, P. (1977). Psychedelics Encyclopaedia. And/Or Press, Berkeley, Ca.
Stevens, J.(1989). Storming Heaven: LSD and the American Dream. London, Paladin Books, pp491-2.
Su, T. P., London, E. D. and Jaffe, J. H. (1988). Steroid binding at s receptors suggests a link between endocrine, nervous and immune systems. Science, 240, 219-223.
Taberner P. V. (1976). The anticonvulsant activity of ketamine against seizures induced by pentylenetetrazol and mercaptopropionic acid. European Journal of Pharmacology, 39, 305-311.
Thomson, A. M., West, D. C. and Lodge, D. (1985). An N-methylaspartate receptor-mediated synapse in rat cerebral cortex: a site of action of ketamine ? Nature, 313, 479 – 481.
Thomson, A. M. (1986). A magnesium-sensitive post-synaptic potential in art cerebral cortex resemles neuronal responses to N-methyl-D-aspartate. Journal of Physiology (London), 370, 531 – 549.
Vaupel, D. B. (1983). Naltrexone fails to antagonise the effects of PCP and SKF 10, 047 in the dog. European Journal of Pharmacology, 92, 269 – 274.
Walker, J. M., Bowen, W. D., Walker, F. O., Matsumoto, R. R., De Costa, B. and Rice, K. C. (1990). Sigma receptors: biology and function. Pharmacology Reviews, 42, 355 – 402.
Westbrook, G. L., Mayer, M. K. (1987). Micromolecular concentrations of Zn2+ antagonise NMDA and GABA responses of hippocampal neurons. Nature, 328, 640 – 643.
Westerberg, E., Monaghan, D. T., Cotman, C. W. and Weiloch, T. (1987). Excitatory amino acid recepors and ischaemic brain damage in the rat. Neuroscience Letters, 73, 119 – 124.
White, P. F., Ham, J.,Way, W. L. and Trevor , A. J. (1982). Pharmacology of ketamine isomers in surgical patients. Anaesthesiology, 52, 231-239.
White, P. F., Schuttler, J and Schafer, A. (1985). Comparitive pharmacology of ketamine isomers. British Journal of Anaesthesia, 57, 197-203.
White, P. F., Way, W. L. and Trevor , A. J. (1982). Ketamine – its pharmacology and therapeutic uses. Anaesthesiology, 56, 119-136.
White, W. F., Nadler, J. V., Hamburger, A.,Cotman, C. W., Cummins, J. T. (1977). Glutamate as a transmitter of the hippocampal perforant path. Nature, 270, 356-357. participate in synpatic transmission following kindling. Nature, 326, 701-703.